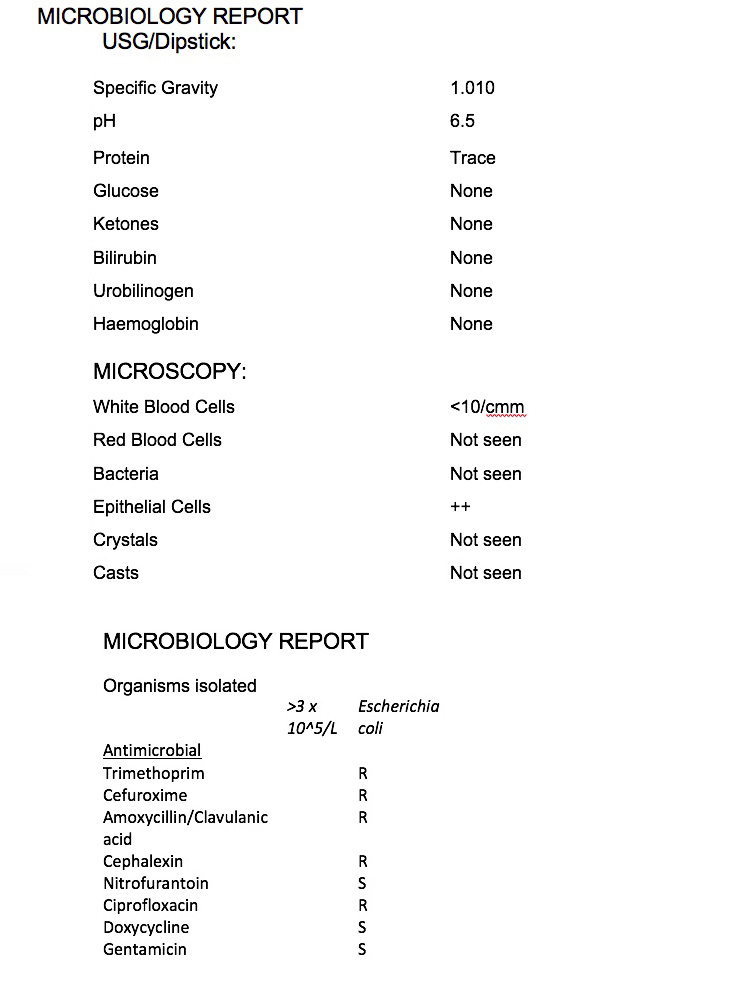
Another dipstick is applied to the urine (as your GP will have done in the surgery) to check for signs of infection or inflammation (white and/or red blood cells, protein and nitrates) including the pH of the urine. Additionally, the dipstick reagent pads test for the presence of Bilirubin, Urobilinogen, Ketones and Glucose.
Urine pH
A neutral pH is 7.0. The higher the number, the more alkaline it is. The lower the number, the more acidic your urine is. The average urine sample tests at about 5.0 as the urine is slightly acidic. This is due to the normal daily acid production in the body to maintain an acid-base balance. Therefore, any abnormalities in the acid-base balance has a direct effect on urinary pH levels.
These levels are particularly useful in the evaluation of stones, crystals or infection. For example, in a patient with a possible kidney stone, the urinary pH level is helpful. The main types of kidney stones are:
- calcium stones, the most common type of stone
- struvite stones, usually caused by an infection, like a urine infection
- uric acid stones, usually caused by a large amount of acid in your urine
Uric acid, cystine, and calcium oxalate stones tend to form in acidic urine, whereas struvite (magnesium ammonium phosphate) and calcium phosphate stones form in alkaline urine.
People with a UTI due to Proteus and Klebsiella bacteria typically have alkaline urine whereas bacteria such as E-coli are usually found in a more acidic environment.
This pH will also be noted on the report. However, pH is also affected by diet; a high protein intake can give rise to acidic urine, whereas a high intake of dairy products or vegetables can give rise to alkaline urine.
White Blood Cells (Leukocytes)
Only a few white blood cells are normally present in urine. When these numbers increase, the dipstick test will become positive. This indicates that there is inflammation in the urinary tract or kidneys and the body is excreting more white blood cells. In addition to possible infection, white blood cells/leukocytes can also indicate chronic kidney inflammation caused by a kidney stone, a tumour of the kidneys, bladder or urethra, infections such as chlamydia or other sexually transmitted diseases and fungal infections such as Thrush.
Protein
Protein in the urine may be a sign of kidney disease. The protein test pad provides a rough estimate of the amount of albumin in the urine. Albumin makes up about 60% of the total protein in the blood. Normally, there will be no protein or a small amount of protein in the urine. When urine protein is elevated, a person has a condition called proteinuria.
Small amounts of albumin may be found in the urine when kidney dysfunction begins to develop. If it is felt necessary the laboratory may request that a further, more detailed urine albumin test be carried out by the GP or hospital. The urine albumin test is more sensitive than a dipstick urinalysis and is routinely used to screen people with chronic conditions that put them at risk for kidney disease, such as diabetes and high blood pressure. Protein in the urine can also be due to dehydration, pregnancy, disease of the heart and some cancers.
Nitrates
Urine will contain a certain amount of nitrate usually down to foodstuffs but, in a normal urine sample, this type of nitrite will be indicated as ‘absent’ or ‘not present’ on a dipstick. But, in certain instances, nitrates can be indicated as being ‘present’ or “+”. The most common occurrence of positive nitrites in urine is in the presence of bacteria which convert the non-ionic nitrate into nitrite.
Bacteria where nitrates would be shown as positive on dipstick include certain species of E. coli, Klebsiella, Proteus or Pseudomonas.
However not all bacteria convert nitrates in the urine so relying on this marker in the testing process does not exclude infection.
An important point to note is the conversion of nitrates in the urine can take up to four hours and a fresh sample of urine may not readily show this if the sample is immediately analysed by the laboratory.
Bilirubin and urobilinogen
Bilirubin is a chemical produced when red blood cells are broken down. It is transported in the blood to the liver, where it is processed and excreted into the gut as a constituent of bile. In the gut, bacteria act on the bilirubin to transform it into urobilinogen. It is usual for urine to contain urobilinogen but not bilirubin. Bilirubin in the urine may be an indicator of a breakdown of red blood cells. It may not be effectively removed by the liver, which may suggest liver disease or a problem with drainage of bile into the gut, such as gall stones.
Ketones
These are chemicals that are formed during the abnormal breakdown of fat and are not normal constituents of urine.
Breakdown of fat may result from prolonged vomiting, fasting or starvation; individuals on a diet or who present with diarrhoea and vomiting may have a positive result.
Ketones can also be present in the urine of people with poorly controlled diabetes. This can make the blood more acidic and is known as diabetic ketoacidosis; it should be reviewed urgently by a doctor. Some medications, such as captopril, may also produce a false positive result (Steggall, 2007).
Glucose
Glucose in the urine (glycosuria) can occur in pregnancy or patients taking corticosteroids. It may also be indicative of diabetes but is not normally found in a urine sample. Although glycosuria is an indication of endocrine abnormality, it is not diagnostic and further investigation, such as fasting blood tests, may be required.