Chronic UTIs develop when ‘acute’ or ‘simple’ infections are left untreated or fail to get better with standard treatments such as over-the-counter remedies or the short courses of antibiotics that GPs usually prescribe.
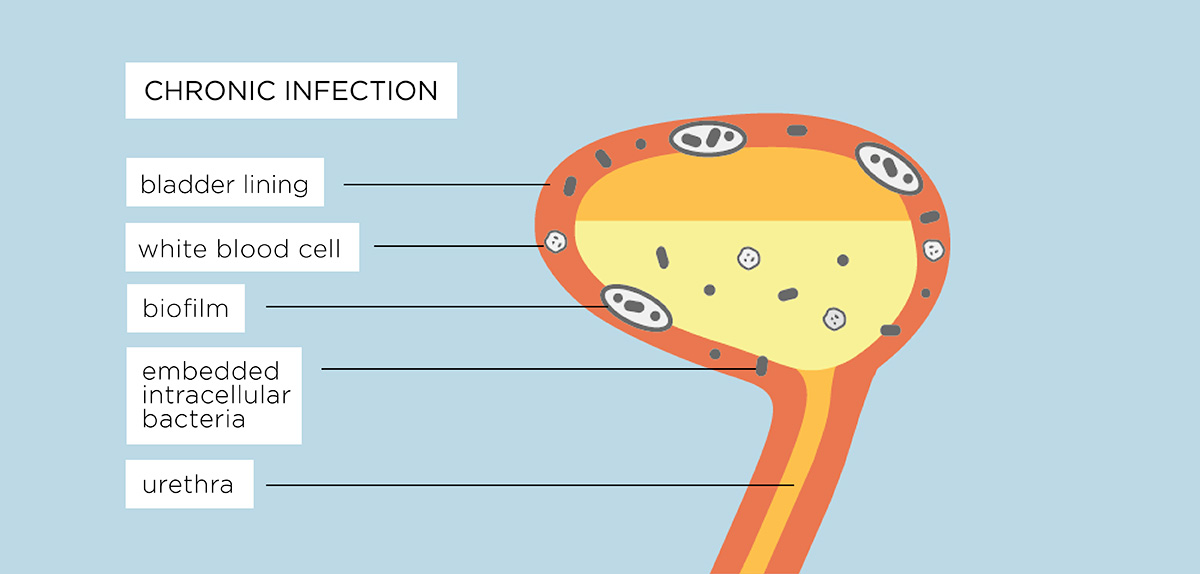
Over time the bacteria that cause UTIs move from the urine and into the cells of the bladder wall where they are protected from antibiotics and become harder to kill. Bacteria cause the bladder cells to become inflamed. This allows the bacteria to ‘stick’ to the tissues and become harder to flush out. We explain below the development of a chronic UTI.
1. Early phase of a urinary infection
The normal bladder is not sterile and contains at least 550 different species of bacteria. It has plenty of microbes – bacteria, fungi and viruses in the urine but they are in comfortable balance with the body and not causing symptoms. But some microbes are pathogens – bacteria that can cause infections or disease. Those suffering an “acute” UTI find a short-course of antibiotics will quickly resolve the infection for around 70% of sufferers. However, for the remainder who do not respond to the prescribed short-course of antibiotics or over the counter remedies, complications begin.
2. Changes to the tissue lining of the bladder
If an infection is not treated correctly, some infection causing bacteria are able to change form and adopt the shape of round cocci – spherical, ovoid or round shape. They can penetrate down to the base of the lining of the bladder and parts of the urethra (the urothelium). Once inside, they hide in the spaces and fluid between cells (interstices and interstitial fluid) or they can invade the cells. This is called intracellular colonisation forming intracellular bacterial communities (IBC).
When these bacteria enter cells they go into a dormant state, similar to hibernation, and so do not divide. They can live in these cells for long periods of time and move into fresh cells – they are called ‘persisters’.
The urothelium is made up of epithelial cells and is about five cells deep. Experts think it takes about 100 days for a cell at the bottom to move to the top.
Persisters are only affected by antibiotic attack when they start dividing, so while they are dormant they survive antibiotic treatments. Short courses of full dose antibiotics kill off large numbers of dividing bacteria in the urine but can’t reach dormant ones.
3. The bladder becomes inflamed
The cells that have become colonised by the infection causing bacteria send distress signals to the immune system, which causes an inflammatory response.
Blood vessels dilate up and cause the bladder wall to look red or inflamed. Some of these blood vessels might burst and leak blood into the urine which will be detected on dipstick analysis or microscopy.
Attracted by chemicals, called cytokines which are released by the infected cells, bacteria start to infiltrate the urothelium (the tissue lining of the bladder and parts of the urethra).
The white blood cells fail to detect a problem because the bacteria are hiding inside the epithelial cells. But the urothelial cells do detect a problem and this standoff results in chronic inflammation and pain.
This inflammation and pain can persist despite apparently ‘normal’ urine results. This is because standard tests look in the wrong place. The bacilli are safe, lying dormant inside the urothelial cells and not in the urine which is collected for tests.
4. Persisting inflammation causes the urothelium to thicken
All epithelial tissue thickens when stressed in any way through a process called metaplasia (think of the skin on your feet).
The tissue lining of the bladder and parts of the thickens as it attempts to form a protective barrier. But it is not very effective – the microbes are already inside the cells.
Both inflammation and the increased number of urothelial cells thicken the wall of the epithelial tissue.
This thickening causes some obstruction which leads to the most sensitive symptom of infection – voiding. Voiding symptoms include hesitancy to pee, a reduced stream, intermittency – stopping and starting, terminal dribbling, post dribbling and double voiding – feeling like you need to go back pee again straight after going.
The thickened and inflamed bladder wall reduces bladder capacity. Inflammatory chemicals can cause the bladder muscle to contract inappropriately. Both cause symptoms like needing to go more frequently, more urgently or urge incontinence – a sudden and strong urge to go.
5. Bacteria that cause disease develop in the biofilm
Biofilms – groups of microbes which come together in a jelly and stick to the inside or outside of cells – are a normal part of our body. They are found all over our body.
But when bacteria that can cause infection and disease get into a biofilm, these bacteria stop dividing and become unsusceptible to antibiotic attack. Bacterial biofilm can be multi-microbial (this means they can contain many different pathogens and species). The now dormant pathogenic bacteria irritate the cells and cause inflammation.These communities are difficult to detect and effectively treat, however, they continue to colonize and modify gene expression utilising behaviours such as quorum sensing which is the ability for bacterial species to transfer behaviours such as antibiotic resistance between each other.
From time to time the pathogenic bacteria can wake up, divide vigorously, burst out the cell and set up fresh infection in new cells.
6. Cells are infected
Pathogenic bacteria escape from shed cells, divide and infect new, fresh cells at the base of the bladder lining.
The body’s natural immune system responds to the infection by shedding the cells. It’s the most effective way of getting rid of the infection.
But the bacteria have detected that they are inside a cell that is dying. They must escape, by waking up and dividing vigorously to create a microbial swarm that bursts out of the cell into the urine.
Continued division causes a ‘planktonic flare’ which can lead to an acute cystitis attack.
7. Persister microbes dormant in the cells of the bladder wall are one feature of a chronic infection
As a persister microbe wakes up it starts dividing. As the cell fills with dividing microbes it becomes damaged and the dividing microbes leak out into the tissue spaces in the bladder wall and some are then shed into the urine as part of the immune system response. This causes an acute flare.
Eventually the cell dies and the microbes continue to divide through the tissue spaces. If they are given the chance they will set up new, dormant, persisters inside fresh cells.
When the microbes are dividing and active in the urine, they are particularly susceptible to antibiotic attack. During a flare, short courses of antibiotics can make immediate improvements only for symptoms to return in a few days or weeks. However, a short course of antibiotics doesn’t tackle the root of the problem – the existence of other dormant persister microbes that are waiting for the right moment to break out of the cells again.
These remaining dormant bacteria periodically send out advance microbes to test the environment and see if it is the right time for them to start growing again.
In this scenario, if the advance microbes sense that the environment is now suitable, they signal the remaining cells to wake up and start multiplying, shedding infected cells, white and red blood cells into the urine, which will result in detectable UTI symptoms via dipstick and mid-stream urine analysis.
However, if the “scouts” bring back bad news, the colony will lay low until the next opportunity and will not be not detectable in dipstick urine analyses because of lower numbers of white blood cells that usually do not meet the diagnostic thresholds applied for acute UTI.
Diagnosing bacterial intracellular/biofilm infections with dipsticks and mid-stream urine tests is next to impossible. Standard urine culture methods do not detect the release of bacterial colonies from single cells shed into the urine so identification of multiple bacteria is not possible. A study published in Urology in 2015 found that 75% of patients with lower urinary tract symptoms (LUTS) had evidence of IBCs compared to 17% found in controls.
What are the symptoms of a Chronic UTI
As a result of the development of a Chronic UTI, people can be left with some or all of the following symptoms. It is important to be aware that symptoms vary from person to person.
- A frequent and pressing urge to pass urine, while only being able to void small amounts of urine. This can rise to 4-6 times an hour on bad days
- Overactive bladder symptoms including urgency, latchkey urgency, waking urgency or incontinence, running water urgency or incontinence and aggravation prior to menstruation.
- Stress urinary incontinence including leakage after laughing, coughing, during exercise or when standing or bending down.
- Voiding problems including hesitancy, an intermittent flow of urine, straining to void, post void dribbling of urine and double voiding
- Pain, usually burning or stinging, when passing urine (known as dysuria) in the bladder or urethra.
- Pain as the bladder fills post voiding or pain that is only partially relieved by urinating or no relief of pain at all after urination.
- Having to get up several times in the night to go to the toilet (nocturia)
- Cloudy urine or blood in the urine (haematuria)
- A strong, sweet or “fishy” smell to the urine – bacteria can change the odour of urine
- For women, pain and inflammation across the pubic bone, pelvic floor and lower abdomen (including the Iliac fossa region). Pain may radiate into the vagina or along the vulva.
- For men, pain and inflammation radiating into the rectum. Pain may travel down the legs as well.
- A pressure sensation in the lower abdomen and pelvis – due to the inflammation of the bladder pressing against the other pelvic organs.
- Fever, feeling generally unwell, a dull ache in the lower abdomen and back. These symptoms may mean the infection has spread to the kidneys
- Emotional distress and brain fog/confusion. This can particularly affect the elderly.
If your acute or recurrent symptoms are now affecting you on a daily basis and you suspect you have a chronic UTI, you can find information about treatment options here