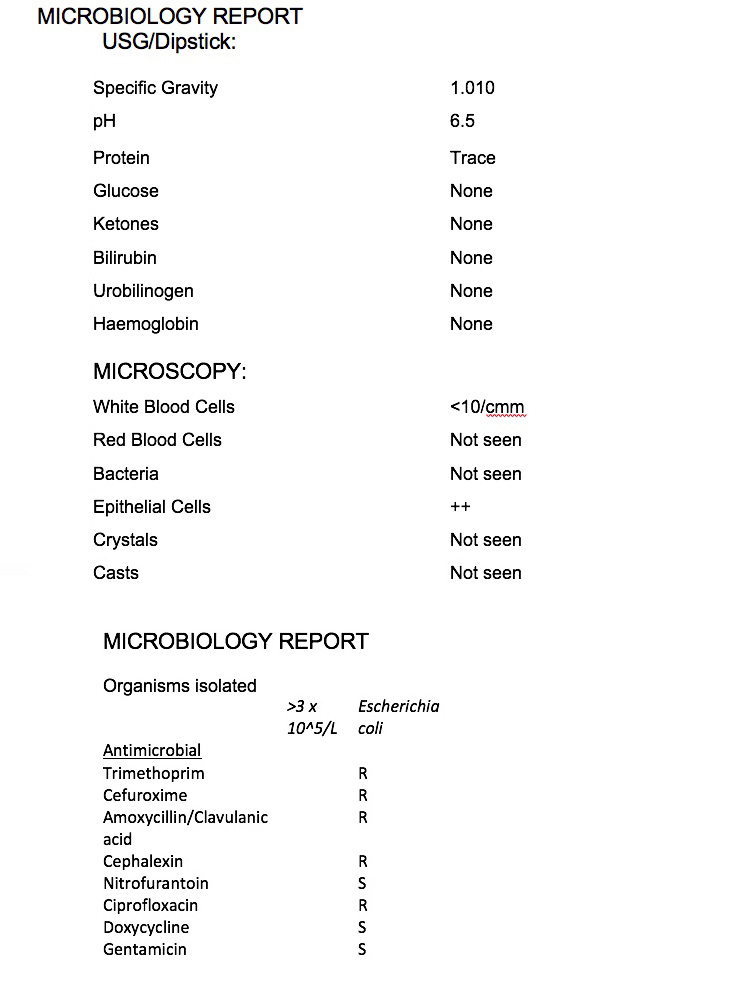
If sufficient bacteria are grown and the single pure strain identified such as e coli or enterococcus, antibiotics will be tested against the bacteria to check their effectiveness in stopping the infection. This is known as susceptibility and resistance and the results will be noted on the lab report to help your GP prescribe the correct antibiotic.
To determine bacterial susceptibility, the laboratory injects the bacteria isolated from the sample into a series of tubes or cups that contain broth dilutions of the antibiotic. After a standardized incubation period, the lowest concentration of antibiotic that prevents visible growth of the organism is classified as the minimal inhibitory concentration (MIC).
The alternate method of bacterial susceptibility is via the disk diffusion method. Using this technique, disk plates are impregnated with various antibiotics and placed on the surface of an agar plate that has been injected with the isolated bacterial sample. The antibiotic diffuses outward from the disk over a standard incubation time, and the diameter of the zone of inhibition is measured. The size of this zone is compared with standards to determine the sensitivity of the organism to the drug.
The laboratory report that will be sent to your GP will report the name of bacterium grown and the sensitivities of the antibiotics tested against each bacterium.
The interpretation of this testing categorizes each antibiotic result as susceptible (S), intermediate (I), sensitive-dose dependent (SD), resistant (R) or no interpretation (NI). What does this mean?
- Susceptible (S): This indicates that the antibiotic may be an appropriate choice for treating the infection caused by the bacteria tested. i.e. the organism is likely to respond to treatment with this drug, at the recommended dosage. Bacterial resistance is absent or at a clinically insignificant level.
- Intermediate (I): It is applicable to those is bacteria that are “moderately susceptible” to an antibiotic. The intermediate category serves as a buffer zone between susceptible and resistant. The antimicrobial agent may still be effective against the tested isolate but response rates may be lower than for susceptible isolates.
- Susceptible-dose dependent (SDD):
This is a new category for antibacterial susceptibility testing. If a particular bacteria falls under this category, the susceptibility will depend on the dosing regimen used. Higher doses or more frequent doses or both should be used to achieve concentration levels that are more likely to be clinically effective. - Resistant (R). If a bacteria is resistant to a particular antibiotic; it won’t be inhibited by that specific medication using a normal dosage. There is also no expectation of this bacteria to respond a higher dosage.
- Non-susceptible (NS) This category is used for bacteria where there are resistant strains.